The Impact and Importance of Quality of Care Measurement
Highlights of the report:
Download a PDF of these Highlights
As reimbursement models evolve towards value-based incentives, quality measurement has become of high importance to health plans and provider organizations. HIRC's report, Quality Measurement: Impact and Importance, provides an overview of health plans' quality metrics initiatives by addressing the following questions:
- How important is quality of care measurement to commercial and Medicare plans?
- Who are the leading quality organizations and what is their perceived credibility?
- Which disease states are most frequently measured with quality metrics, and which metrics are utilized? How will this evolve?
- How are health plans approaching quality-based reimbursement with network physicians?
- What opportunities exist for manufacturers to collaborate with managed care organizations on quality-related initiatives?
Key Finding: Payers favor manufacturer offerings that align with the plan's quality measurement goals and seek expertise and support from pharmaceutical firms to keep abreast of Medicare star and HEDIS "moving targets."
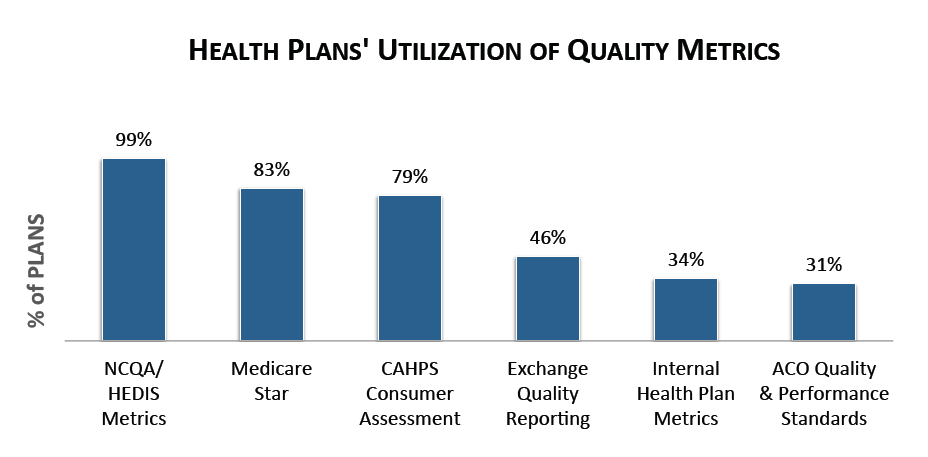
HEDIS Metrics Are Utilized Most Frequently by Health Plans to Measure Quality of Care, Followed by Medicare Star. Quality metrics are developed by a variety of organizations, and health plans may develop their own internal quality guidelines as well. Health plans report most commonly utilizing HEDIS metrics to measure quality of care, citing that they are widely accepted, nationally recognized standards. Nearly 83% of health plans use Medicare Star measures and about 79% of plans utilize the CAHPS consumer assessment to measure patient satisfaction.
The complete report provides greater detail on health plans' internally-developed quality metrics, information on quality organizations, and health plan panelists perspectives on the importance of quality and credibility of various quality organizations.
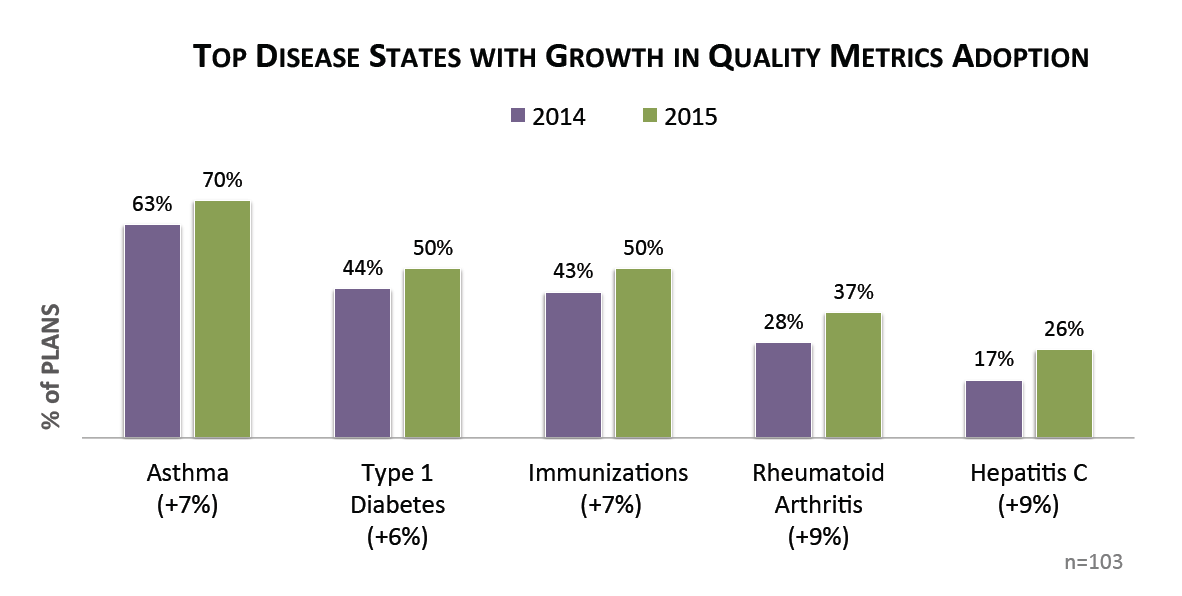
Health Plans Report Greatest Increase in Quality Metrics Adoption for Rheumatoid Arthritis and Hepatitis C. While the prevalence of quality measurement across most disease states held steady from 2014 to 2015, health plans have increasingly adopted quality measures in specialty therapeutic areas, such as rheumatoid arthritis and hepatitis C. An additional 6-7% of plans report adopting quality metrics for common chronic disease states in 2015, namely asthma and type 1 diabetes. Quality measurement in the immunizations space also demonstrated an increase in 2015.
The full report provides an overview of health plans' use of quality metrics across more than 20 disease states currently, as well as what is expected by 2018. Detailed profiles for the following top measured disease states are provided:
- Asthma
- Atrial Fibrillation
- Breast Cancer
- Colorectal Cancer
- Congestive Heart Failure
- COPD
- Coronary Artery Disease
- Depression
- End-stage Renal Disease
- Hematological Cancers
- Hyperlipidemia
- Hypertension
- Immunizations
- Prostate Cancer
- Rheumatoid Arthritis
- Type 1 Diabetes
- Type 2 Diabetes
Research Methodology and Report Availability. In December-January, HIRC surveyed 70 commerical health plan quality managers and pharmacy and medical directors. Thirty-three Medicare executives were also surveyed. Online surveys and follow-up telephone interviews were used to gather information. The Quality Measurement: Important and Impact report is part of the Quality of Care: Models and Metrics Service, and is now available to subscribers at www.hirc.com/summary/qcmm.
Download a PDF of these Highlights
Download Full Report (Subscribers only) >

