Health Exchange Plans: Access, Quality Measurement, and Care Management
Highlights of the report:
Download a PDF of these Highlights
Enrollment in Health Insurance Marketplace plans is projected to increase notably by 2016. Understanding plan approaches to quality measurement and care management is critical to forming strategic partnerships in this growing market segment. HIRC’s report, "Health Exchange Plans: Quality and Access Perspectives," addresses the following questions:
- How are plans using formulary and benefit design to manage medication costs? What are the management implications for commercial populations?
- How do exchange carriers expect provider networks to evolve? How do they approach provider reimbursement?
- How are exchange plans addressing quality and care management for their exchange populations?
- Which manufacturers have best engaged plans in exchange-specific issues? What are the trends in contracting for the exchange?
Key Finding: Exchange plans are managing chronic disease through case management, care management, and quality initiatives. Opportunities for partnership include medication adherence support and competitor best practices sharing.
Novo Nordisk, Merck, and Boehringer Ingelheim Lead in Exchange Plan Engagement. Novo Nordisk received the highest ratings from pharmacy and medical directors representing carriers in state-based and federally-facilitated exchanges, followed by Merck and Boehringer Ingelheim. Rankings are based on a cumulative score in company presence with exchange plans, account management support regarding exchange-specific issues, willingness to contract, and engagement in quality and care management issues.
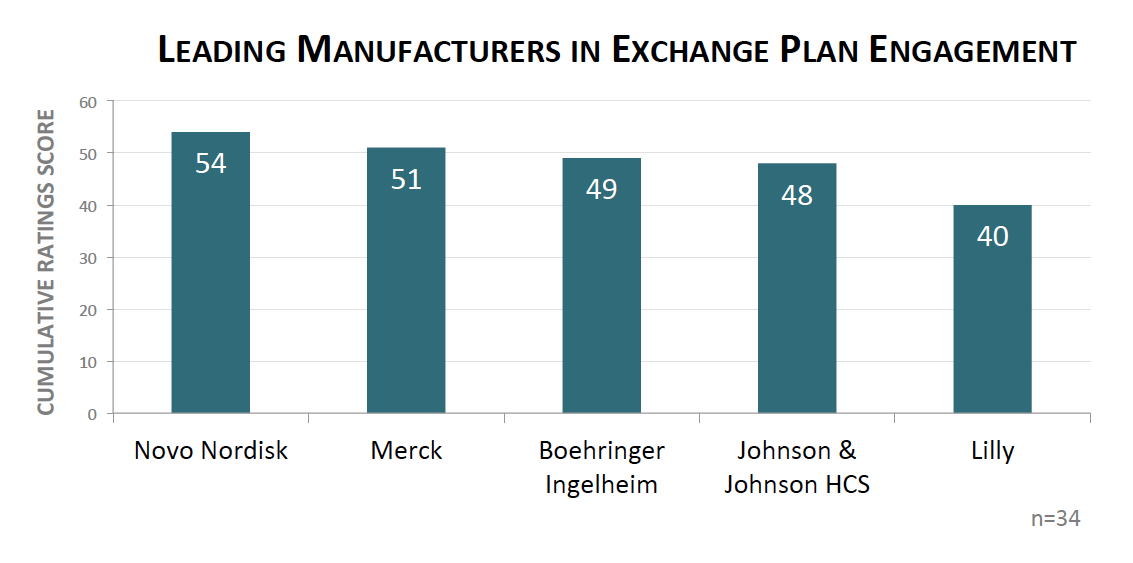
The full report provides ratings for the top 20 manufacturers meaningfully engaging exchange plans, and profiles for select manufacturers.
Quality of Care Measurement of High Importance to Exchange Plan Carriers. Health plans report that quality measurement in their exchange populations is extremely important. In beta testing for 2015, the Health Insurance Marketplace Quality Rating System (QRS) will have future implications for how plans are evaluated on performance and quality, and how plans adjust their care management program offerings. In addition to QRS, plans report utilizing HEDIS metrics and CAHPS surveys to measure quality among exchange members.
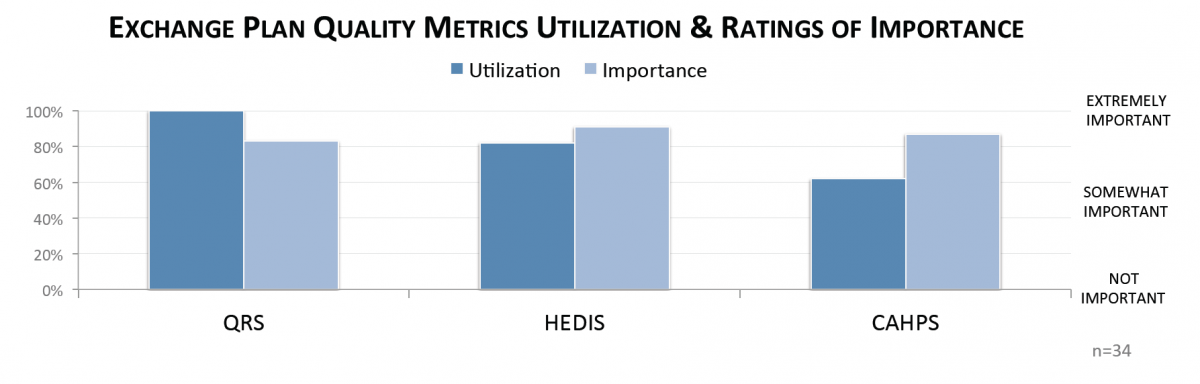
The full report provides results of in-depth follow-up interviews with health plan decision-makers, where perspectives and anticipated challenges to quality measurement for exchange members are explored.
Payers' Needs in Medication Adherence Presents Opportunity for Manufacturer Partnership. While most plans report that their approach to care management for exchange populations mirrors that of commercial, follow-up interviews suggest that nearly half expect to adapt their care management offerings for exchange members in the next 1-3 years. Panelists cite adherence support tools as the greatest unmet need in care management for their exchange population.

Research Methodology and Report Availability. In December-January, HIRC surveyed 34 pharmacy and medical directors from plans operating in the federally-facilitated and state-based exchange, representing 3.4 million lives (43% of the public exchange market). Online surveys and follow-up telephone interviews were used to gather information. The State Health Exchanges: Quality and Access Perspectives report is part of the Quality of Care: Models and Metrics Service, and is now available to subscribers at www.hirc.com/summary/qcmm.
Download a PDF of these Highlights
Download Full Report (Subscribers only) >

